My Heart Will Go On: Heart Arrhythmia and Running

I’m writing this because I found so little information in going through my encounter with a heart issue brought on by (or perhaps brought to light by) my long-distance running life. I hope this can be an encouragement to endurance athletes who encounter arrhythmias or sinus node irregularities.
I was training for the 2024 Houston Marathon. This marathon was my fourth training cycle and it would have been my third marathon. (I had to scratch the Chicago marathon with a hamstring injury through which I ran too long.) I was a month out from Houston. My coach assigned me Yasso’s 800s. This is a tough workout that is meant to predict your marathon time. The average of what you can do in 10 800s with about equal time rest after each rep is supposed to give in minutes and seconds what your marathon time would be in hours and minutes. My average was under 3:30. I was psyched since this predicted a 10-minute+ PR.
The next day I went for an easy five-mile recovery run and found myself light-headed, very slow, and with a soaring heart rate. Of course I still finished the five miles. I was supposed to run 22 miles the next day (for those concerned, I had re-arranged the long run to be earlier in the week, I didn’t usually run long two days after a hard workout) and I asked my coach if I should still try. She told me to hydrate well and try in the morning thinking that the issue was due to dehydration.
One of the things I have learned from this whole situation is that I need to be much more willing to respond by taking time off. I need to be less responsible to the schedule. I don’t think I should have tried to do that 22. But I did. I could only do 9 miles, and my heart rate soared to over 180. I had to call my husband to come get me. I still walked about a half mile to a good pick-up stop. I don’t know if that was a great idea. Anyway, heart rate came down eventually. I thought maybe I had a cold because I was coughing and trying to catch my breath that day and the next. The third day I went for a run, and you guys–it was great! The first mile still found my heart rate high, but it came down and I was running easy sub-10s, and I ended up doing five miles, I think. The next day I ran 8 miles up and down Spokane’s South Hill. I was slower, but I was running hills, so I didn’t think anything of it. The next day I didn’t run because of the weather and the day after I ran for about a mile when I felt dizzy again. And the roads were icy so it wasn’t ideal conditions. The next day I had an easy run, and it was fine. The day after that I ran a long 16 and it was slow-ish but fine. Then an easy day, and then I did a hard workout of 5 x 6 minutes at half-marathon goal pace. The last six minutes felt hard on my lungs and chest, but hey that’s marathon training, right? But the recovery day after that I felt fainty again. I couldn’t run a mile. At this point, my coach told me she thought I should go to the doctor.
I’ll save you the rigamarole of the primary doctor, but I’ll just say, I think I should just see specialists only. I didn’t feel like the primary care doctor was really very helpful at all. I think they have a protocol that is basically an algorithm and they don’t have the capacity to see patients as individuals. This same doctor accused me of drug-seeking when I complained of sciatica pain; she gave me a prescription for Prilomax when I complained of gut discomfort heartburn (which for all I know was early signs of this heart issue); and she regularly dismisses my suggestion that various issues are perimenopause related. I now have an appointment with an internist to change my primary care provider, but getting that appointment took some doing and it isn’t until October. I did learn from tests the GP ordered I had low ferritin so I thought that was the culprit. I got an Apple Watch that does wrist EKG’s and sent some that seemed weird to a cardiologist friend and he said I had junctional beats. This cardiologist friend thought maybe I had an upper pulmonary infection that was prompting the high heart rate; the junctional beats seemed more an issue for a low heart rate. I did get into a cardiologist, had more bloodwork done, and an exercise test and a heart monitor put on.
The Monday before I saw the cardiologist for the first time I ran on the treadmill for three easy miles and it was glorious. At the end of that run, my heart rate did soar. But it didn’t feel like it was and I tried not to look. But I haven’t done that since because the cardiologist seemed a little agnostic about whether that would be ok. I have been lifting. Let me just say that the waiting and the not being able to easily go for a run and the possibility that maybe I can’t run made me sad and worried. I love to run. I love the feeling of being out on the roads. I love to push my body and see that it is able to do what I set for it. But when my body is not doing what I ask it to do, I’m really frustrated. I worried that I did this to myself. Maybe I didn’t eat enough or get enough iron, magnesium, or potassium — all possible culprits people suggested to me.
I’ve listened to and read extensively about the ways women are treated by the medical establishment as small men and the way that athletes pose difficulties to the diagnostic process for doctors who don’t typically see athletes. I think what might seem like normal low-end numbers on tests are in fact actually low in a problematic way for athletes, especially around iron-related numbers like hemoglobin. I really thought those could be the issues and that people weren’t paying attention to what mattered.
The Hospital and the Catheter Ablation
But then… the day after I had the monitor put on, I relocated for the semester to Lubbock, TX, where I am the inaugural scholar-in-residence at the Humanities Center at Texas Tech. I had the monitor installed on Monday and on Saturday I went for a run. I wore my Apple Watch 9 series and kept the HR on. After a half mile, my HR was soaring to the 170s, so I stopped and walked for a half mile and it came down so I ran another 3 miles and it was fine. Then I walked around the block. I was so happy that I seemed to be back running. The next day, I walked to a coffee shop a mile away with a friend and then walked back. When I got back, my heart rate was at 120 and it wouldn’t come down. So I thought, this is a problem, I should go to the ER. A friend drove me to the ER and when I got there they did an EKG right away and the EKG showed atrial flutter. I sat in the ER for six hours, and then they decided to admit me. I got there around 2:30 or 3 PM and I was moved to a hospital bed around 9. I had come out of the flutter without a conversion, at which point my heart rate could be quite low and then swing to very high for a short time and then it would come back down.
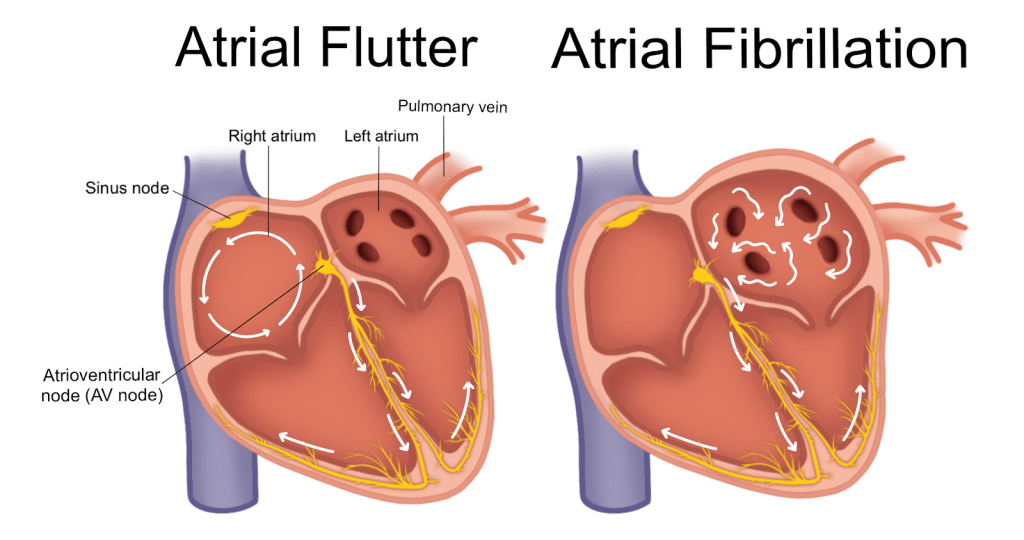
Atrial flutter is an arrythmia in which the current is stuck in a circuit and it won’t stop. They solve this problem by burning places along the circuit so that the current cannot continue. The scarring becomes the block to the current so that it can’t jump and returns to normal. That’s what my heart was doing, but it came out of it on its own. It isn’t as bad as atrial fibrillation, which puts you at risk of stroke.
So they admitted me. The nurse in the first ward I was admitted to told me that runners think that low heart rate is always good but that isn’t necessarily true — the heart aims toward 60 and that is best. Around 3 AM, as I was trying to sleep, I felt myself fall off. Four nurses rushed into the room. They said that my heart had stopped beating for 5.5 seconds. Then a nurse told me that they were worried about me falling asleep because they weren’t sure they could tell the difference between me being asleep or in a coma. Needless to say, that did not help my sleep.
Because of the heart pause, they moved me to cardiac ICU. They didn’t put me on any drugs — except a painful shot of a blood thinner — because I wasn’t in an arrhythmia. The next day the electrophysiologist (EP) came and told me I had atrial flutter and they were more worried about the high rate part of my telemetry than the low rate. They said it was not life-threatening and that they could do a catheter ablation which would solve the issue. The junctional beats seemed to be coming about because the one node was jumping ahead of the other when the heart rate was too low, but they thought that addressing the flutter would solve that too. I had the procedure early in the morning, general anesthesia with intubation and all. That hurt my throat for a couple days afterward. The whole procedure was done in an hour. They shaved my pelvic area after I was out, went in through my right groin, right where the leg meets the pelvis, stuck a wire in a vein threaded to my heart and then sent heat through the wire to burn places in my heart to break the electrical circuit. They told Jeff that they burnt 14 places. When I got back my HR was closer to 60s. But now my sitting heart rate still seems to be regularly below 50.
At ten days out my chest and my groin at the point of insertion were a little sore, but by a month the point of entry was beginning to fade. In the hospital, they were eager to have me return to an active running life, but nine days after the procedure was the first time I really even walked very far. I walked over 2 and a half miles through the airport and felt pretty good about it. I had a follow-up appointment on March 7, when the electrophysiologist (EP) set me up with a heart monitor for a month. I was still having junctional beats, some chest pain, and I would have periods of light-headedness up until about the middle of March, which would have been six weeks since the ablation.
Two Months Out
After I had been wearing the heart monitor for about a week, I received a frantic phone call from an on-call nurse on a Sunday about the pauses the heart monitor was catching. She advised me to come in, but I was at home in Indianapolis and not in Lubbock where I was continuing cardiology care. So I didn’t go in. I did have pauses every day. The cardiologist’s office called me four days before I was to remove the monitor and return it. The EP had said that they got the information they needed and they wanted me to send it back so they could look at everything at once. Meanwhile I returned to running. I ran longer and I started doing some speed work (first 12 x and then 18 x 100s). The second time I did feel tightness in my chest — if I had stopped after 12 I am sure I would have felt better.
At my follow-up appointment six weeks after the last visit, which was almost eleven weeks since the ablation, I learned that the ablation worked. The flutter is gone. But I do have a peculiar sinus node. The pauses are due to the sinus node, but they do not appear to have biological causes. The EP thinks I should be able to return to regular running. Issues I am having now are probably from deconditioning and from the psychological issues of learning to trust myself again and of being hyper-attuned to heart rate. I did have one post-run issue that the monitoring company read as atrial fibrillation, but my doctor thinks is not necessarily afib. He thinks it was just from post-cardio tachycardia. He said the strips were very noisy there so it looked like I was running. I’ve also begun to wonder if the 3200 feet above sea level might affect me here in Lubbock. I have been traveling and I ran hills in Providence, RI and Seattle and that felt good.
Take-Aways
The EP’s NP told me that I didn’t do anything to bring this on, but I suspect that low iron, low magnesium and low potassium (they worried about my magnesium and potassium numbers while I was in the hospital, gave me several big doses of potassium, and put me on a magnesium drip) all contributed to stressing my heart and bringing on the atrial flutter. The EP also told me that I would probably deal with body trust a bit going forward, and he repeated that at our last appointment. That makes sense to me. I think it is a matter of worrying about whether my body will hold up through hard efforts. About five weeks out I ran four miles at sub-9 pace with an average of 127 HR based on my Polar 10. Now at 11 weeks out I’m trying to be more careful and run slower, but it was nice to know that was possible. I have also started doing some mild speed workouts over the last four weeks. Last Monday I did 200s and they were hard, but I think it might have been the heat and the fact that I had just been at sea level and was running at 3200 feet.
So here is what I want to say about all this in relation to running. I found all kinds of ways to avoid taking this seriously and I want to encourage people who run seriously to have a cardiologist. Chest pain is chest pain — you might have heartburn, but it might also be your heart. These symptoms cannot be wholly addressed with iron, magnesium, and potassium, although maintaining those minerals is important and the lack of them can trigger problems. The solution can’t just be to supplement. Almost everyone I talked to who was an experienced runner downplayed this situation. Even my exercise test didn’t catch the problem. If you suspect you have atrial flutter, don’t let them end the stress test just because you are in shape — make them go until they push you into the arrhythmia. Get a heart monitor as soon as it happens so that they can catch the arrhythmia. And then if it happens and won’t come down, go to the ER. If it keeps happening and keeps coming down, ask the cardiologist to consider an ablation.
I have been working on this post since I went into the hospital. I haven’t posted it because I wanted to offer an ending. The ending I want is a PR at a marathon, but that is probably going to take a little while, so I’m going to go ahead and post and I will update when I’ve run the next race. Keep your heart healthy, friends. Run happy.